Main Type of Skin Cancer — Their Differences, Histology and Prevention.
Introduction
Since I started my medical studies in Townsville, Queensland, Australia, I have always heard that Queensland is the "skin cancer capital of the world". Curiously I thus decided to look into this claim.
Through epidemiological studies, Queensland has the highest age-standardised incidence of melanoma 64.3 compared to 48.7 per 100,000 nationwide (RACGP, 2014). Interestingly, Australia comes second to New Zealand, as they are the number 1 country globally with an age-standardised incidence of melanoma 50.3 per 100,000 nationwide (Whiteman et al, 2016). Melanoma is an aggressive and lethal skin cancer that can cause death if not treated promptly.
Townsville's UV index at noon between September to April is always around 10-12 (which is very high), and for only a few months, from May towards August, the UV index ranges between 6-8. From my personal experience, I can always feel a more distinct 'sting' when I am exposed to the Queensland sunshine. I was always aware of keeping my shirt on and putting on the right amount of suns-cream/sunscreen.
So why is there so much skin cancer in Australia? There are a few reasons for this, such as a culture to love the outdoors (strong sense of sports, barbecue, beaches, et cetera), a population with European descendants that has fair skin which is not suitable for the harsh sun, proximity to the equator (high UV index), a country with a sunny climate, the earth's elliptical orbit around the sun (which increases UV by about 7%) and a low pollution zone that does not artificially block the UV radiation.
The outcome of prolonged exposure to a UV radiation (all depends on time and intensity of exposure) causes sunburns, leathery skin, accelerated aged skin and damage to the skin cell DNA, which leads to cancer and potentially death.
Quick facts & epidemiology
Australia and New Zealand have the world's highest incidence rate for melanoma. Incidence rate means the number of new cases within a time period as a proportion of the number of people at risk for the disease.
Skin cancer (melanoma and non-melanoma) is the most common cancer diagnosed in Australia.
About two in three Australians will be diagnosed with some form of skin cancer before the age of 70.
Almost 980,000 new cases of basal cell carcinoma (BCC) and squamous cell carcinoma (SCC) are treated each year.
Melanoma is the third most common cancer diagnosed in Australia and is more commonly diagnosed in men than in women.
The risk of being diagnosed with melanoma by age 85 is 1 in 13 for men compared to 1 in 22 for women.
1,375 deaths due to melanoma skin cancer were accounted for in 2020 in Australia, where melanoma accounts only for 1-2% of all skin cancers. 679 deaths due to non-melanoma skin cancer were accounted for in 2016 in Australia.
There is a 92% chance of surviving a melanoma tumour that was caught early.
Data from Cancer Council Australia, Australian Bureau of Statistics Causes of Death Report, Australian Institute of Health and Welfare.
The basic skin anatomy
Figure 1: Demonstrates the basic skin layers.
From: Cancer Council Victoria.
The skin, part of the integumentary system, helps the body by protecting the internal organs from the outside world, regulate body temperature, making us waterproof, prevent loss of body fluids, use our sensory nervous system to feel the world (pain, temperature, pressure), excrete some waste, hold some fat storage, play a role with the immune system and synthesise vitamin D.
The skin can be divided into three layers. The first most superficial layer is the epidermis (epi from the Greek aetiology meaning on, upon, over. Hence, epidermis = on the dermis). The epidermis contains squamous cells, basal cells and melanocytes (there are other more cell types). The squamous cells are essential as they are the cells that are in contact with the world. They are tightly packed together and flat. They make up the thickest area of the epidermis and overtime shed itself. The basal cells are cubed-like cells and are at the bottom of the epidermis layer. They continuously multiply, and as they age, move upwards to become flat squamous cells. The melanocytes are within the layer of the basal cells. They produce melanin, through a process called melanogenesis, which is a dark pigment that provides the skin colour. These pigments absorb the UV-B light and prevent it from being absorbed in the layers below. Thus, harmful UV light cannot damage or break any DNA, which could potentially cause cancer.
The dermis sits below the epidermis. This layer contains all the essential supporting functions for the dermis such as the lymph vessels, vasculature, nerves, hair follicles and glands as well as the matrix/elastic (collagen and elastin architecture) which support the epidermis needs to be anchored to the dermis. Below the dermis is the subcutaneous layer or hypodermis or the fat layer. The hypodermis anchors the dermis with loose connective tissue and holds fats for storage, insulating and for energy use. Larger blood vessels can be found here as well as a strong immune presence.
What is cancer?
Cancer cells are mutated cells that have lost the tight control of replication, repair and the normal cell death function. The DNA is found to be faulty, which is a crucial step in oncogenesis (onco meaning tumour or mass, and genesis meaning origin or source). Having acquired too many mutations results in the cancer cells to use specific techniques to stay alive successfully. These mutations contribute to the ‘hallmarks of cancer’ which describes the behaviour and techniques that cancer cells utilise. These are:
Hide and avoid the immune system.
Enabling replicative immortality, meaning cancer cells do not become old or do not have a set amount of replication like normal cells.
Sustaining proliferating signalling indicating the cancer cells can proliferate without any external stimuli.
Evading growth suppressors means that cancer cells manage to not respond to molecules that would stop or inhibit proliferation.
Resisting cell death.
Inducing angiogenesis, meaning that cancer cells promote the formation of a vascular system to nourish itself.
Activating invasion and metastasis, meaning cancer cells are able to go from one organ to another.
Deregulation of cells energetics, meaning that cancer cells change the cell internal reaction to favour itself.
Promoting inflammation and favouring genome instability and mutation.
The outcome of cancer cells on the body is: damage to nearby organs due to its growth (such as pinching neurons or pushing against the brain), loss of organ function (for example if cancer grows on the heart muscles, the muscle will be weaker and loses its original function), using crucial resources away from normal cells, releasing of certain hormones at an inappropriate amount which acts on the body, promotes inflammation which causes damage and unusual immune response which may attack healthy cells.
Nomenclature of neoplasia - the basics
Before we go on about describing skin cancers, we need to understand how they are named. To name a particular cancer, a prefix and a suffix is required, where the prefix describes the tissue type, and the suffix describes either benign/malignant. ‘Oma’ means benign tumours whereas ‘sarcoma or carcinoma’ means malignant tumours, bear in mind that malignant tumours are generally known as the more aggressive and invasive tumours. The difference between sarcoma and carcinoma is that sarcoma comes from the mesenchymal tissue (bone, muscles, cartilage) and the carcinoma comes from the epithelial origin (skin).
Here are some examples:
Fibro + oma = fibroma means benign tumour arising from fibrous tissue.
Osteo + sarcoma = osteosarcoma, malignant cancer arising from mesenchymal tissue (bone in this case).
Squamous cell + carcinoma = squamous cell carcinoma, malignant cancer arising from epithelial tissue.
Unfortunately, the naming system has some exceptions such as melanoma which would mean melanin + oma = melanoma, meaning benign cancer arising from melanocyte cells (melanin-producing cells). However, melanoma is a carcinoma of melanocyte cells, hence should actually be called melanocarcinoma. There are lots of exceptions, and the nomenclature (system of names used in a particular specialist field) of cancer is long and descriptive; hence in this blog, we are only doing those that describe what is relevant.
Difference between Basal Cell Carcinoma, Squamous Cell Carcinoma and Melanoma
There are three main types of skin cancers, and these are the basal cell carcinoma (BCC), squamous cell carcinoma (SCC) and melanoma. BCC and SCC are malignant epidermal tumours (coming from the epidermis of the skin) and are known as non-melanoma skin cancer. BCC and SCC are strongly linked with ultraviolet (UV) exposure, where an increase in exposure leads to an increase in BCC and SCC emergence. BCC and SCC are both locally infiltrating cancers, but it is important to note that there is a low risk of metastasis and most are not life-threatening (do bear in mind they can still cause death if they metastasise). BCC and SCC can cause disfigurement (if it is left to be grown and not surgically removed) and may leave large scars once surgery is done. Melanoma, arising from melanocytes, is the most dangerous and aggressive skin cancer, and should be treated as soon as possible. The outcome depends on how much a melanoma has infiltrated its local surrounding, which describes the percentage chance of the tumour to have metastasised (such as the more a melanoma tumour has infiltrated, the more chance it has reached a blood vessel and spread to other organs).
The risks and causes of developing BCC, SCC and melanoma tumours are due to UV exposure (intensity and duration), tanning beds, previous diagnosis of skin tumours, skin type (fair/tan, eye colours, hair colours), outdoor working, and a history of childhood of sunburns/tanning. Melanoma risks are amplified by family history, increased number of unusual moles, a depressed immune system and previous diagnosis of melanoma skin cancer. Interestingly, solariums (sun-beds) are banned in Australia, and it was found that those who have used solariums below the age of 35 have almost a 60% greater risk of developing melanoma cancers in their lifetime.
It is worthy to note that the molecular and genetic basis for BCC, SCC and melanoma are not very well understood. However, in BCC, the PTCH1, which is a tumour suppressor, is lost. In SCC, there is a TP53 loss of function (also a tumour suppressor) and there is a gain of function with RAS. In melanoma, the mutations include BRAF, RAS, TP53, PTEN and CDNK2A. A quick note: tumour suppressors are crucial genes to, as the name suggest, suppress any formation of tumours by repairing the DNA within the cells or committing apoptosis (safe and control cell death). RAS is a gene that controls cell growth, differentiation of the cell and cell survival. If there were to be a gain of function of RAS, a cell would start to proliferate uncontrollably to which it can metastasise. Hence, tumour suppressors and controlled proliferation genes are essential for humans not to get cancers.
Basal Cell Carcinoma
Basal cell carcinoma is the most common skin cancer of them all. BCC accounts for about 70-80% of the non-melanoma skin cancers. It originates from the lower layer of the epidermis. Since BCC is strongly related to UV exposure, you generally find them near the scalp, face, neck, shoulders and back but can appear anywhere on the body. There are no symptoms when a BCC develops, and it develops quite slowly (months to years) generally without spreading or metastasising to other organs. If it does spread, lymph nodes, lung, bones are its preferred sites. May be locally destructive and disfiguring if left to be grown.
Gross appearance: have many types of characteristics. The most common colours are reddish tan, pale to bright pink, pearly white or skin colour, or may be a brown, black or blue lesion. May be a nodule or papule with a raised lesion that has “pearly” edges or a pearl lump. May sometimes be scaly with dryness or be eczema-like, and may be shiny/waxy. The patch may ulcerate, bleed and fail to heal. Often with telangiectasia (tiny blood vessels cause threadlike red lines or patterns on the skin).
Microscopic appearance: basaloid cells with scant cytoplasm and elongated hyperchromatic nuclei. Apoptotic bodies and mitotic figure present. There is stromal mucinous alteration, peripheral palisading and peripheral clefting may all be present. Focal keratinisation may be noticed. Secondary features such as inflammatory reactions, amyloid deposition or dystrophic calcification may be present.
Figure 2: Demonstrates BCC as reddish tan to pink/pearly papules or nodules, with or without central ulceration. Often with telangiectasia.
From: Pathology Outlines.
Figure 3: Micrograph of basal-cell carcinoma, showing the characteristic histomorphologic features (peripheral palisading, myxoid stroma, artefactual clefting). H&E stain.
From: Nephron on Wikimedia Commons.
Squamous Cell Carcinoma
Compared to BCC, SCC originates from the upper layer of the epidermis. SCC is also considered as non-melanoma skin cancer. The same can be said about SCC as it is also strongly related to UV exposure where you generally find them near the scalp, face such lips, nose and eyelids, ears, neck, shoulders, back of the hand and lower legs, but can appear anywhere on the body. SCC develops quickly over a few weeks and months without spreading or metastasising to other organs. Signs include a thickened red, scaly spots or a sore that has not yet healed. May be rapidly growing lump and may be tender to the touch. SCC may spread if left untreated and if it does spread, the lymph nodes, lung, bones are its preferred sites.
Gross appearance: displays variable degrees of differentiation and cytological features. Often hyperkeratotic erythematous scaly/crusted plaques, papules, nodules or ulcers. May have induration, ulceration, haemorrhage. May be whitish, pink or brown.
Microscopic appearance: keratinocytes carcinoma may have infiltrated the dermis. Precursor lesions are often present. Depending on the differentiation there could be no/minimal keratinization, focal keratinization or marked nuclear atypia. May be difficult to establish squamous differentiation. The histology is quite challenging as there are many histologic patterns with variants. It is interesting to note that on the histologic spectrum of SCC, they all share downward growth which is below the level of the adjacent or overlying epidermis.
Figure 4: Demonstrates the scaly red areas that may bleed easily. Sore-looking that does not heal.
Figure 5: Demonstrates an invasive well-differentiated squamous cell carcinoma. Notice the keratinising tumour is infiltrating the dermis.
From: Shaofeng Yan, M.D., Ph.D., Pathology Outlines.
Melanoma
Compared to BCC and SCC, melanoma is more aggressive and lethal. Melanoma accounts for 1-2% of skin cancers and can spread/metastasise to other organs in the body. The outcome of metastasising is an increase in mortality, and a decrease in treatment effectiveness. Melanoma tumours are also found to be resistant to radiotherapy. The risks of developing melanoma are due to UV exposure (intensity and duration), tanning beds, previous diagnosis of melanoma tumours, family history, the amount of melanin (skin type, eye colour and hair colour) in an individual and a depressed immune system. They can develop all over the body but are mostly found on the face, neck, shoulders, arms and back. It is worth noting that melanoma has been found on the sole of the feet, palms of the hand, inside the eyes and under the fingernail beds. Melanoma tumours can grow from weeks to months. Melanoma can come from existing moles on the skin (doesn’t have to be a mole) or the unusual growth on the skin or an unusual pigmentation development. There are no apparent symptoms, but the first signs are the changes in a mole or existing pigment, or unusual skin growth.
For example:
The colour of a mole may change or become blotchy.
The size of a mole may become bigger.
The shape of a mole may become irregular or may increase in height or a raised area may develop.
Itching, pain or bleeding can present itself.
If the melanoma does metastasise it will go towards the brain, lungs, liver, adrenal glands, bones, gut and other parts of the skin. Secondary melanoma may be asymptomatic (without symptoms) until the tumour becomes large and cause noticeable damage. The 5 and 10-year survival rate for a melanoma that did not metastasise is 97% and 93% respectively. The 5 and 10-year survival rate for a melanoma that did metastasise is 53% and 39% respectively.
Gross appearance: the ABCDE method can be utilised. An asymmetrical/irregular shape with possible irregular/uneven borders may be noticed. The diameter may be more than 6 mm and may change colours as well as growing/evolving. Colours such as blue whitish veil, greyish-blue areas and black/brown dots may be noticed. There could be irregular extensions and branched streaks. Central ulceration may present itself.
Microscopic appearance: just like the SCC, the histology is quite challenging as there are many histologic patterns with variants. It is also dependant on the level of differentiation and invasion. DermNet NZ shows detailed pictures of the growth of melanoma tumours. However, we can summarise melanomas as asymmetrical and poorly circumscribed lesions with architectural disturbance and usually marked cytological atypia (variation from normal). DermNet NZ describes the melanoma histology as a “consumption of the epidermis, pagetoid spread of melanocytes, nests of melanocytes with variable size and shape (which may be confluent and lack maturation), melanocytes within lymphovascular spaces, deep and atypical mitoses and increased apoptosis”. Ulceration, if present, is a poor prognostic factor. Mitotic figures are common.
Figure 6: Demonstrates a melanoma. Notice the first signs where it has changed from being a mole (such as changes in size, shape and colour). There are variations with an irregular border. The diameter may be more than 6 mm.
From: MayoClinic, Melanoma.
Figure 7: Demonstrating a melanoma tumour in situ by using Melan-A staining.
From: DermNet NZ.
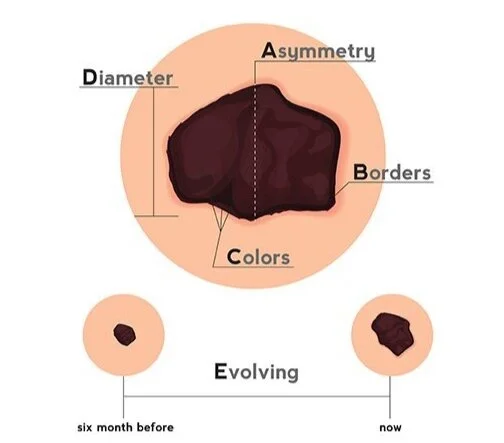
ABCDE
Figure 8: Demonstrates the ABCDE method.
From: Cone Health.
Due to melanoma being the most lethal skin cancer and arising from moles or suspicious growth or unusual pigmentation, the ABCDE method was implemented for anyone to quickly assess any unusual development. It is always a good idea to check your body for any of these criteria and mention to your doctor. See Spot the Difference with Cancer Council Australia.
(A)symmetry
Look for any irregularity. Divide the spot into two and notice if it is mirrored or not.
(B)order
Look for any irregular edge or an edge that is difficult to define.
(C)olour
Notice the colour and how many colours you can see. Is it uniform and are there spots identified?
(D)iameter
The diameter should be less than 6 mm to be normal. If it is more than 6 mm, you should be a concern.
(E)volving
Notice changes in colour, shape, border or diameter. Is it bleeding, inflamed, oozing? Does it struggles to heal? An evolving mole is concerning.
Intervention of BCC, SCC and Melanoma
Diagnosing
If you notice anything suspicious and used the ABCDE method, your GP or dermatologist may use a biopsy where the sample is examined under a microscope from a pathologist. A biopsy is essential to accurately distinguish between skin cancers. The biopsy helps in identification (thus in the diagnosis of the cancer) and is useful for cancer staging by using the TNM method (which describes the stages of cancer). By identifying which cancer it is (non-melanoma or melanoma), the treatment can then be chosen, and prognosis can be estimated from similar previous data.
See BCC and SCC what to expect and Melanoma what to expect for patients that go through the initial investigation, treatments and outcomes.
Treatment
Biopsy
Most of the time, the cancer is completely removed when a biopsy is done. This is generally enough for BCC and SCC tumours as a treatment.
Surgery
A method used to remove cancer with its surrounding tissues to make sure all the cancer cells have been removed. This method is done under local anaesthesia. BCC and SCC generally do not require any further treatments.
Radiotherapy
Can be challenging to apply as skin cancers such as melanoma are resistant to radiotherapy. This method utilises electrons or photons to kill cancer cells by harming their DNA and creating free radicles. Radiotherapy is used when surgery may not be a choice and is used for areas that are hard to reach, such as eyes, nose and forehead. Radiotherapy may be used for metastasised cancers and reduce/kill other cancers in other organs (which can enable surgery if the tumour has shrinked in size).
Chemotherapy
BCC and SCC can be treated through topical creams that contains drugs that kills cancer cells. Useful for the most superficial cancers or pre-cancerous cells that has been noticed (which may become cancers). If cancer has metastasise (such as stage 4), then chemotherapy will be used to kill other cancers in other organs by using intravenous delivery.
Immunotherapy
A biological therapy such as using monoclonal antibodies (MAb) that are very specific to act on certain cells, receptors or activating the immune system. Lately, this technology is expanding and becoming more and more efficient.
Other treatments
The use of cautery (burning), curettage (scraping off), cryotherapy, and photodynamic therapy may all be used.
Prognosis
The prognosis depends on the cancer staging using the TNM method and the general health and age of the patient. Statistically speaking, BCC and SCC are treated successfully. Melanoma tumours are more aggressive, and the prognosis is heavily dependent on the staging. An important clue is the thickness of invasion in the local skin. These are described below and are more related with melanoma tumours:
Stage 0 is less than 0.1mm,
Stage I less than 2mm,
Stage II greater than 2mm,
Stage III spread to lymph nodes and
Stage IV distant spread.
In melanoma, ulceration was found to predict a poor outcome. At early-stage melanoma, surgery will most likely be the course of outcome where about 1-2 cm of skin is removed to make sure all the melanoma tumour cells are removed. If the tumour has spread to the lymph nodes, the removal of those lymph nodes will most likely be the course of action. Advanced melanoma is stage 4, where cancer has spread to other organs. The aim of stage 4 is to suppress and control cancer from causing damage, discomfort or death. At this stage, it is about improving the quality of life for the patient. Surgery, chemotherapy, radiotherapy, biological therapy (immunotherapy) and targeted therapy are all therapies that may be used. Palliative care is introduced when the patient is nearing the end of their life, hence providing the most comfortable death transition is regarded to be the best outcome.
Prevention
The good news is that skin cancer is 100% preventable and should always be mentioned with your doctor when visiting. The following are steps you can take to minimise harmful UV light exposure, intensity and duration. This is not to say completely hide and live in the dark, but all sunlight intake should be in moderation and thought of. After-all we do need sunshine to create vitamin D. The UV light, being a critical factor and risk, thus should be minimised into a safe amount of sunshine intake. Think: Slip, Slop, Slap, Seek and Slide.
Use loose-fitting clothes (Slip). Clothes are better than suns-cream at stopping sunlight from reaching the skin. They may be uncomfortable when swimming with it, hence get light and specially made clothes for the sea.
Use a quality suns-cream with a good environmental impact (Slop). It is recommended to get SPF30+ sunscreen that protects from UV-A and UV-B (broad-spectrum). Get a water-resistant suns-cream.
Get a hat to cover the head (especially the scalp), nose, ears and neck (Slap).
Avoid sunburns by limiting sun exposure that has a UV index above 3, especially in the middle of the day. Here, in Queensland (Australia), the UV index is considered high (near 10-12 at noon) for the whole year-round. Look out for the local UV alert before leaving.
(Seek) shade when resting or having a picnic, but bear in mind that UV radiation can bounce on surfaces (such as concrete, sand, snow); hence you are still exposed to some UV radiation.
Use sunglasses to protect the eyes (Slide).
Use the SunSmart application (it is free).
For patients at high risk, using the ABCDE and yearly consultation with a dermatologist is recommended. Many skin cancers can be detected by people themselves or from a family member. Make sure to look everywhere on the body, which includes scalp, back, soles of the feet, back of the legs and back of the neck. Do not ignore any spots and make sure to use proper lighting. In case of any doubts, seek your GP for a skin check.
For those working outdoors or in the workplace that is exposed to sunlight, see the Work oudoors? pamphlet from the Cancer Council Australia.
Myths to think about
“It is cold, and the clouds will protect me”. You can still get sun damage on windy, cloudy or cool days. Temperature does not affect the amount of UV you are exposed to.
“A fake tan darkens the skin, thus protecting the skin from the sun”. This is found not to be accurate as you still need protection.
“Cosmetic products protect me from UV radiation”. Yes, some cosmetics are protective if labelled as such but may not be as effective as regular suns-scream. It is recommended to apply suns-cream every 2 hours.
“People with dark/olive skin are not at risk of skin cancers”. The skin still needs care and protection regardless of the amount of melanin involved. You are always at risk! People with darker skin are indeed more naturally protected and resistant to UV radiation than people with fair skin. Hence, check out which Fitzpatrick scale you are on.
“SPF50+ allows me to stay in the sun a lot more than SPF30+”. This is an interesting thought. SPF50+ sunscreens filter about 98% of UV whereas SPF30+ filters about 96.7% of UV radiation. They are both sufficient and protect you from the UV if applied every 2 hours. It is recommended to use SPF30+ or higher. People get the idea that the SPF50+ is enough to be applied once for the whole day, which is incorrect. Applied once is never enough if you have a whole day of UV exposure.
“I need the sun for vitamin D”. Vitamin D does not require intense exposure to the sun. A typical person with a UV index of 3 or higher will get the amount of UV exposure for vitamin D synthesis by doing everyday activities such as walking to the car/shops. Interestingly, the body has a daily limit in creating vitamin D; thus, extra exposure does not increase vitamin D but does increase the risk of skin cancer. A few minutes is all it takes.
“Skin cancer is not a concern as you can see it and treat it easily these days”. Having done my surgical rotation, I can guarantee you that skin cancer such as BCC/SCC(s) have been found in obscure areas. They can sometimes be tough to spot. Melanomas have been found in spots that get almost no UV exposure. Always bear in mind that skin cancers can be invasive, they can leave scars behind, and they can kill you. Surgery, chemotherapy and radiotherapy may be needed to treat skin cancer as it is not always a simple excision. Remember, 2,000 people die every year in Australia from skin cancer.
“Only people who tan or seek the sun get cancer”. Actually, overexposure to the sun can happen at outdoor work, gardening, picnic, jogging/walking, driving long distances et cetera.
Tanning easily or not burning from the sun (compared to other people) does not mean you are safer from getting skin cancer. It is a sign of skin trauma if the skin darkens, even if there is no peeling or redness. The skin darkens by adapting to the UV exposure it is exposed to.
Be mindful when driving. Sun exposure can cause harm and increases the risk of skin cancer.
Published 15th July 2020. Last reviewed 25th April 2022.
Reference
Allan J Pollack, Mark McGrath, Joan Henderson, Helena Britt. Skin cancer by state and territory. Royal Australian College of General Practitioners website. https://www.racgp.org.au/afp/2014/august/skin-cancer-by-state-and-territory/. Published August, 2014. Accessed July 12, 2020.
Australian Institute of Health and Welfare. Melanoma of the skin. Australia Government: Cancer Australia. https://melanoma.canceraustralia.gov.au/statistics. Updated July 7, 2020. Accessed July 12, 2020.
Cancer Council Authors. Factsheet. Cancer Council website. https://www.cancer.org.au/content/pdf/Factsheets/MS%20214%20CCA%20MELANOMA%20POSTER%20V4%20.pdf. Accessed July 11, 2020.
Cancer Council Authors. Melanoma. Cancer Council website. https://www.cancer.org.au/about-cancer/types-of-cancer/skin-cancer/melanoma.html. Updated January 13, 2020. Accessed July 11, 2020.
Cancer Council Authors. Non-melanoma Cancer. Cancer Council website. https://www.cancer.org.au/about-cancer/types-of-cancer/skin-cancer/non-melanoma.html. Updated January 22, 2020. Accessed July 11, 2020.
Ghassan A. Tranesh, M.D., Hong Qu, M.D. Basal Cell Carcinoma. Pathology Outlines website. http://www.pathologyoutlines.com/topic/skintumornonmelanocyticbcc.html. Updated May 31, 2020. Accessed July 11, 2020.
Christopher S. Hale, M.D. Melanoma. Pathology Outlines website. http://www.pathologyoutlines.com/topic/skintumormelanocyticmelanoma.html. Updated March 27, 2020. Accessed July 11, 2020.
Mayo Clinic Authors: Basal Cell Carcinoma. Mayo Clinic website. https://www.mayoclinic.org/diseases-conditions/basal-cell-carcinoma/symptoms-causes/syc-20354187. Updated September 14, 2019. Accessed July 11, 2020.
Mayo Clinic Authors: Melanoma. Mayo Clinic website. https://www.mayoclinic.org/diseases-conditions/melanoma/symptoms-causes/syc-20374884. Updated March 10, 2020. Accessed July 11, 2020.
Mayo Clinic Authors: Squamous Cell Carcinoma. Mayo Clinic website. https://www.mayoclinic.org/diseases-conditions/squamous-cell-carcinoma/symptoms-causes/syc-20352480. Updated June 21, 2019. Accessed July 11, 2020.
Shaofeng Yan, M.D., Ph.D. Squamous Cell Carcinoma. Pathology Outlines website. http://www.pathologyoutlines.com/topic/skintumornonmelanocyticscc.html. Updated January 13, 2020. Accessed July 11, 2020.
The American Cancer Society medical and editorial content team. What Are Basal and Squamous Cell Skin Cancers. American Cancer Society website.
https://www.cancer.org/cancer/basal-and-squamous-cell-skin-cancer/about/what-is-basal-and-squamous-cell.html. Revised July 26, 2019. Accessed July 11, 2020.
WebMD Authors, Stephanie S. Gardner, MD. Basal Cell Carcinoma. WebMD website. https://www.webmd.com/melanoma-skin-cancer/melanoma-guide/basal-cell-carcinoma#1. Reviewed November 2, 2018. Accessed July 11, 2020.
WebMD Authors, Stephanie S. Gardner, MD. Skin Cancer. WebMD website. https://www.webmd.com/melanoma-skin-cancer/melanoma-guide/skin-cancer#1. Reviewed March 3, 2020. Accessed July 11, 2020.
WebMD Authors, Stephanie S. Gardner, MD. Squamous Cell Carcinoma. WebMD website. https://www.webmd.com/melanoma-skin-cancer/melanoma-guide/squamous-cell-carcinoma#1. Reviewed February 12, 2019. Accessed July 11, 2020.
Whiteman DC, Green AC, CM Olsen. The Growing Burden of Invasive Melanoma: Projections of Incidence Rates and Numbers of New Cases in Six Susceptible Populations through 2031. J Investig Dermatol. 2016;136(6):1161-1171. doi: https://doi.org/10.1016/j.jid.2016.01.035
ADDITIONAL SOURCE OF INFORMATION:
For health professionals: what the RACGP recommends from the Red Book.