An Introduction to Alzheimer's Disease with Its Normal Anatomy and Its Pathophysiology.
Introduction
Around the world, there is a need to increase the expenditure in development and research of dementia (1). Statistically every 3 seconds, one person is developing dementia which 60-70% of the cases are diagnosed as Alzheimer’s disease (AD) (1,2). Another worrying fact is that the number of people with AD will triple by 2050 (1). The latest World Alzheimer Report has demonstrated that there are not enough publications of neurodegenerative disorders and compared to cancer publications there is an astounding 1:12 ratio (1). It is also noted that there are not enough people going into dementia research as there has not been any significant breakthrough in the past 40 years (1).
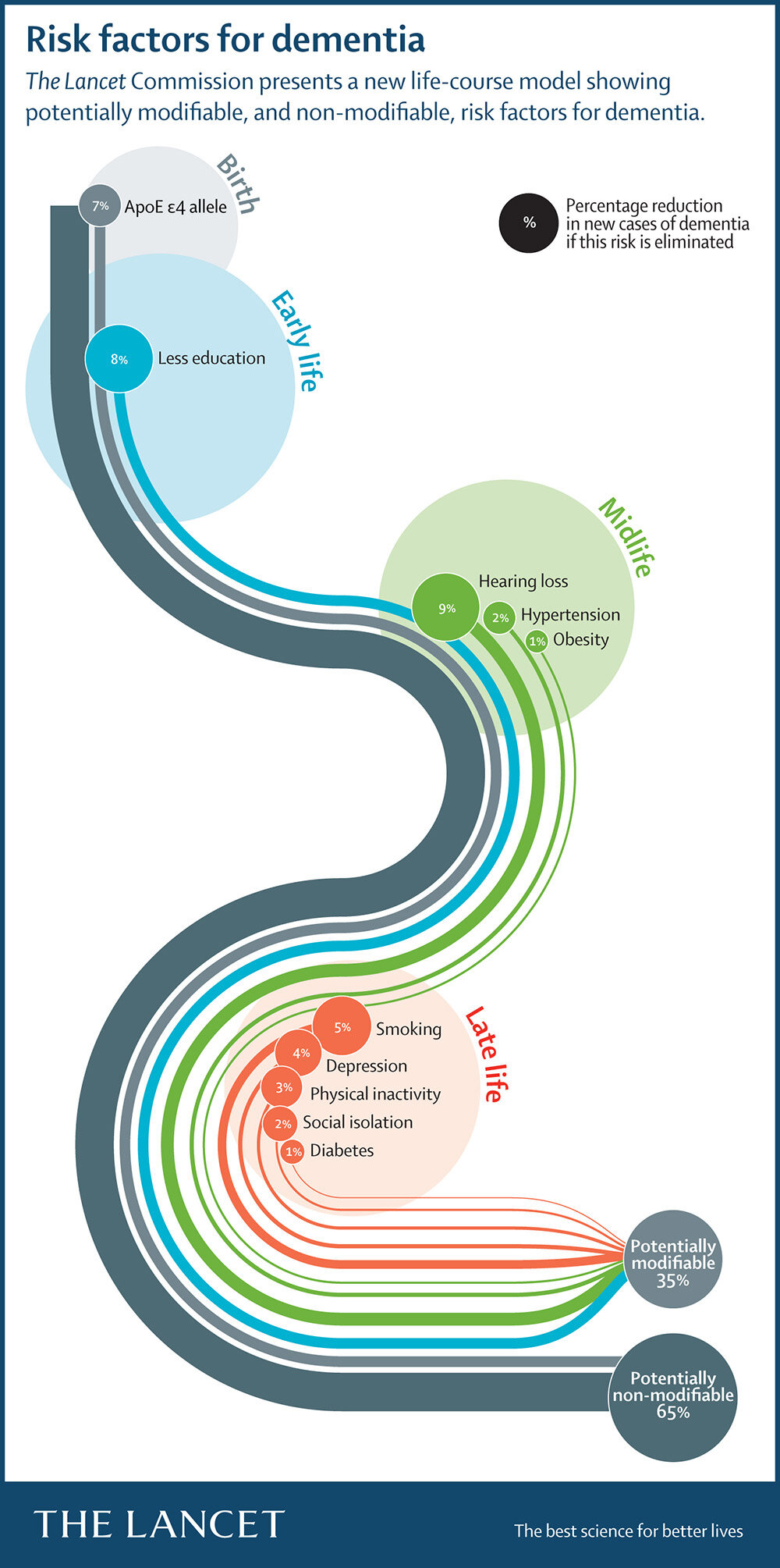
In the United States, as the population age increases, there has been a significant increase of 145% in Alzheimer’s death whereas it has been reported that the number one cause of death (heart disease) has decreased by 9% (3). Currently, there are different approaches to treat and alleviate AD and its symptoms. These treatments focus on sleep change, behaviour change, alternative medicine and most important medications for memory, intellect, rationality and social skills (4-7). Out of these, the medications for memory are the most relevant, the least developed and have the lowest available options. These represent only four drugs which are the cholinesterase inhibitors (donepezil, rivastigmine and galantamine)(8) and memantine(9), a partial antagonist of N-methyl-D-aspartate (NDMA) receptor (3). Ultimately, the main goal is to stop the unknown and current known reasons why neurons are dying in the brain. Hence, where the medication is most needed it is unavailable as there are no drugs to prevent nerve cell death. At the moment we can focus on reducing the modifiable risk factors of dementia which represents a modest 35%. 65% are non-modifiable risk factors where genes take up only 7% and what makes up the other 58% is still a mystery (10).
In the meantime, where humanity is awaiting for a breakthrough, there has been a Whole Person Focus approach for people who are suffering from AD where the Wicking Dementia Centre in Tasmania is brilliantly achieving.
What you can do about dementia
the Massive open online course (MOOC)
The MOOC is done through the Wicking Dementia Research and Education Centre, which is through the University of Tasmania, Australia. Two courses are free and are 4 and 7 weeks long respectively. The 7-week course is about ‘Understanding Dementia’ and the second course (4 weeks) is about ‘Preventing Dementia’. I think they are available twice a year so go ahead and sign up to get started! Here is the link: Understanding Dementia (MOOC), look for the Enrol or Enter Course.
Why enrol? I believe that the facts are up-to-date and recent. The courses are very relevant especially to people who work in health, or people who know someone with dementia or going through themselves with dementia. I recommend these courses and as a medical student, I feel it has improved my understanding of dementia especially on the focus of the person which is extremely important.
Hence, if you know someone who has been affected or is going through with dementia then try this free online course as awareness and education is really important.
Below is the Understanding Dementia is a Massive Open Online Course (MOOC) through the University of Tasmania:
From the University of Tasmania website: “Understanding Dementia is a Massive Open Online Course (MOOC), offering university-quality education about the latest in dementia research and care. This free course provides an opportunity to engage with the perspectives of an international community, without requiring exams or assignments.
Understanding Dementia is designed to be accessible and appealing to people from diverse backgrounds, including:
Health professionals, community and residential facility support staff, people in the early stages of the disease, their families and carers, social scientists, health policymakers and individuals with a general interest in dementia.”
The normal anatomy and physiology
Let us start from the beginning with the basics. The body is controlled by the master controller which is the nervous system. The nervous system is made up of 100 billions of cells called neurons and enables us to interact and influences us with the world such as thinking, planning, memory making, sense and respond to our environment, homeostasis inside the body and perform complex functions from the ‘higher-order’ (11). The nervous system also gives us our unique behaviour and personalities (11). As a whole, the nervous system is organised in two major parts. That is the central nervous system (CNS) and the peripheral nervous system (PNS). The CNS includes the brain which sits in the skull and the spinal cord and the PNS is described as branches coming out from the spinal cord towards glands and muscles. With the PNS there is a two-way communication which allows voluntary and involuntary control and sensation.
The nervous system is extremely complex but can be seen as a highly connected network of cells which can adapt and change with experience and can, to a certain limit, regenerate from injury (11). Each neuron is connected with another neuron and each connection is called a synapse (12). A synapse is a structure which permits an electrical and chemical signal, through dozen different types of neurotransmitters (such as acetylcholine or glutamate), to be transmitted to another neuron (12,13). This has many complicated steps that ultimately let neurons transfer complex information to each other. There are about 100 trillion synapses, each transmitting complex information (12).
According to the ‘use it or lose it’ principle, there are more connections when new skills are learnt such as learning a new language or doing crosswords. This is called neuroplasticity, where the brain can change and develop the connections (11). The same can be used if a child was brought up with a deprived stimuli environment where it is shown to have 25% fewer synapses (11). Hence, building connections through neuroplasticity creates a ‘cognitive reserve’ which provides alternative routes for information to flow (12). It is extremely important to have a high cognitive reserve which helps when there is a pathology causing disruption such as dementia (12,13).
The pathophysiology of Alzheimer’s Disease
Dementia is a spectrum of symptoms which declines the brain function (14,15). This interference affects a person to not be able to carry out a normal social life and will eventually die from related symptoms (14-16). AD represents about 2/3 of dementia cases and is described as a neurodegenerative disease where neurons slowly and irreversibly die over time (16). Ultimately, the disease leads to nerve cell death and the loss of tissues in the brain which over time shrinks the brain affecting nearly all functions (14-16). Scientists are not sure of the reason why the neurons are dying (14,16).
At a microscopic view, the prime suspects for neuron cell deaths are the build-up of plaques which are abnormal clusters of protein fragments and the dying nerve cells containing twisted strands of proteins called tangles (14)
The plaques are proteins pieces that are chemically sticky called beta-amyloid (Aβ) proteins that have clumped together and surrounds the nerve cells (14,16). It is thought to directly damage or have a toxic effect on the neurons and their surroundings (16). Interestingly the Aβ protein is a normal protein that the brain produces and clears all the time (16). Although researchers still do not quite understand its normal function, it may be important for synaptic transmission and communication.
In AD, the Aβ proteins stick together and form an abnormal filament, self-aggregate and form a spherical plaque (14,16). Originally the pieces come from bigger proteins found in the fatty membrane which surrounds the nerve cells. These Aβ plaques block cell-to-cell from signalling one another and may activate an immune response which triggers inflammation (14). Millions of these plaques can occur and result in disabled and damaged neurons on top of degeneration of synaptic connections (14,16). Figure 1 below demonstrates how these plaques are formed.
Figure 1. Formation of beta-amyloid proteins into plaque-like structure (16). Image taken from the Massive Open Online Course: Understanding Dementia.
The neurons utilise a vital cell transport system which is made of proteins called the cytoskeleton (14). The cytoskeleton also offers shape and support. These transport systems are parallel and orderly-like delivering key materials to the cell. A certain protein called tau keeps the vital strands straight (14,16). However, in AD the tau protein is somehow abnormal and collapsed, twisting the strands (now called neurofibrillary tangles) and stops the vital supplies (14,16). The straight strands disintegrate into a ball-of-wool like structure, and the cell eventually dies and wither away leaving a tombstone or a ghost tangle as the tangles are highly insoluble (14,16). Unlike the plaques, the neurofibrillary tangles occur within the cells and again it is the transformation of a normal protein into the abnormal protein behaviour. Figure 2 demonstrates how ghost tangles/tombstones are formed.
Figure 2. Formation of neurofibrillary tangles within the neuron cells leaving ghost tangles or tombstones (16). Image taken from the Massive Open Online Course: Understanding Dementia.
Overall, there are a lot fewer connections and signalling being made between neurons at the synapses and there are a lot of less healthy neurons available which influences signalling (14,16). There is a substantial deficit in cholinergic neurotransmitters (such as acetylcholine), increased oxidative stress and an imbalance in the homeostasis of metal ions (16).
The plaques and tangles tend to be predictable when spreading through the brain, but the rate of the progression varies. The progression depends on other health conditions, age at diagnosis and the stage of the AD (14,16). In the earlier stage, there are no symptoms and no test to detect it. The plaques and tangles start to build up in two regions in the brain which includes thinking/planning and learning/memory and in particular the hippocampus which helps in developing new memories (16).
The mild to moderate AD stage impacts the memory, thinking and planning where they are developing more plaques and tangles. This causes individuals to develop memory and thinking problems which interfere with work and social life. As such they get confused with handling money, organising thoughts and expressing themselves (16). Generally, that is when individuals get diagnosed. Personality and behaviour may also change as well as having difficulty in recognising familiar family members. At this stage, the plaques and tangles are now spread to areas which involve speaking/understanding speech and the sense of body relation to objects (16).
In the last stage, the majority of the brain has shrunk and is damaged due to cell death. Individuals cannot communicate, has no awareness of what is going on, recognise loved ones, care for themselves and are often lying in bed or a chair (14). In the end, physical function such as respiration rate, feeding, swallowing is affected and tends to lead towards recurrent pneumonia which is the final cause of death (14,16).
Novel drug treatment
See the upcoming blog titled “Novel Drug Treatment for Alzheimer's Disease.” for exciting new drugs that will hopefully be on the market and make a difference in Alzheimer’s disease!
Conclusion
Alzheimer’s disease, the most common form of dementia, is a major public health concern. There are no cures for Alzheimer’s disease and there is a lack of medication that can stop the disease’s progression. Currently, there is only palliative therapy with patient-centred care approach. There is a lack of research, publications and funding in Alzheimer’s disease. However, scaffolding techniques with unique linkers which increased drug effectiveness, interesting new insights on old drugs and serendipity sheds a light of hope towards curing Alzheimer’s disease.
Abbreviations
Aβ Beta-amyloid
AChE Acetylcholinesterase
AD Alzheimer’s disease
CNS Central nervous system
NDMA N-methyl-D-aspartate
PNS Peripheral nervous system
Published 20th October 2019. Last reviewed 1st December 2021.
Reference
1. Patterson C. World Alzheimer Report 2018: The state of the art of dementia research, new frontiers. Alzheimer’s Disease International website. https://www.alz.co.uk/research/WorldAlzheimerReport2018.pdf. Published September, 2018. Accessed August 29, 2019.
2. World health organization. Dementia. World health organization website. https://www.who.int/news-room/fact-sheets/detail/dementia. Updated May 14, 2019. Accessed August 29, 2019.
3. Alzheimer’s Association. 2019 Alzheimer’s Disease Facts and Figure. Alzheimer’s Association website. https://www.alz.org/media/documents/alzheimers-facts-and-figures-2019-r.pdf. Published 2019. Accessed August 29, 2019.
4. Wicking Dementia Research and Education Centre. Medical management: Part 1. [Video]. Massive Open Online Course (MOOC). https://mooc.utas.edu.au/course/content/17-56. Updated 2019. Accessed July 15, 2019.
5. Wicking Dementia Research and Education Centre. Medical management: Part 2. [Video]. Massive Open Online Course (MOOC). https://mooc.utas.edu.au/course/content/17-57. Updated 2019. Accessed July 15, 2019.
6. Dementia Australia. About Dementia: Drugs Treatment and Dementia [Internet]. 2016 [cited 2019 August 29]. Available from: https://www.dementia.org.au/files/helpsheets/Helpsheet-AboutDementia09-DrugTreatmentsAndDementia_english.pdf.
7. Dementia Australia. Drug Used to Relieve Behavioural and Psychological Symptoms [Internet]. 2016 [cited 2019 August 29]. Available from: https://www.dementia.org.au/files/helpsheets/Helpsheet-DementiaQandA04-DrugsUsedToRelieveBehaviouralAndPsychologicalSympoms_english.pdf.
8. Dementia Australia. Drug Treatments for Alzheimer’s Disease – Cholinesterase Inhibitors [Internet]. 2018 [cited 2019 August 29]. Available from: https://www.dementia.org.au/files/helpsheets/Helpsheet-DementiaQandA01-CholinesteraseInhibitors_english.pdf.
9. Dementia Australia. Drug Treatments for Alzheimer’s Disease – Memantine [Internet]. 2016 [cited 2019 August 29]. Available from: https://www.dementia.org.au/files/helpsheets/Helpsheet-DementiaQandA03-Memantine_english.pdf.
10. Frankish H, Horton R. Dementia Prevention, Intervention, and Care. The Lancet website. https://www.thelancet.com/commissions/dementia2017. Published July 19, 2017. Accessed September 5, 2019.
11. Wicking Dementia Research and Education Centre. The Nervous System: Part 1. [Video]. Massive Open Online Course (MOOC). https://mooc.utas.edu.au/course/content/17-18. Updated 2019. Accessed July 15, 2019.
12. Alzheimer’s Association. Inside the Brain: A Tour of How the Mind Works. Part 1: Brain Basics. Alzheimer’s Association website. https://www.alz.org/alzheimers-dementia/what-is-alzheimers/brain_tour. Updated 2019. Accessed August 29, 2019.
13. Wicking Dementia Research and Education Centre. The Nervous System: Part 2. [Video]. Massive Open Online Course (MOOC). https://mooc.utas.edu.au/course/content/17-20. Updated 2019. Accessed July 15, 2019.
14. Dementia Australia. What is Dementia? Dementia Australia website. https://www.dementia.org.au/about-dementia/what-is-dementia. Updated 2019. Accessed August 30, 2019.
15. Alzheimer’s Association. Inside the Brain: A Tour of How the Mind Works. Part 2: Alzheimer’s Changes the Whole Brain. Alzheimer’s Association website. https://www.alz.org/alzheimers-dementia/what-is-alzheimers/brain_tour_part_2. Updated 2019. Accessed August 30, 2019.
16.Wicking Dementia Research and Education Centre. Pathology of Dementia: Part 1. [Video]. Massive Open Online Course (MOOC). https://mooc.utas.edu.au/course/content/17-20. Updated 2019. Accessed August 15, 2019.